Speaking the Same Language and Delivering the Best Care as a Team at End of Life
Providing an end-of-life-care curriculum to the University of Arizona’s four health professional schools—Medicine, Nursing, Pharmacy and Public Health– will ensure that every health professional student graduating from the UAHS has basic competency in serious illness and will be able to compassionately care for Arizona’s diverse population. This ambitious undertaking would not have been possible without the support and leadership of Michael Dake, MD, Senior Vice President UA Health Sciences, and Associate Vice President Dan Derksen, MD, who brought all four schools together to create an aligned vision. Dr. Dake has also committed to embedding the training in each school’s curriculum and sustaining it beyond The David and Lura Lovell Foundation grant. “This Lovell support helps catalyze one of the key components of our strategic plan pillars – Healthy Aging – led by Drs. Fain and Insel,” said Dr. Dake.
Dr. Derksen added, “Arizona ranks second (to Florida) for retirees moving to the state. Since 2010 Arizona’s over age 65 population grew 48% versus 34% in the US overall. This curriculum will help us train our health professions students about healthy aging and prepare them to provide compassionate end-of-life care in partnership with their patients and their patients’ families.”
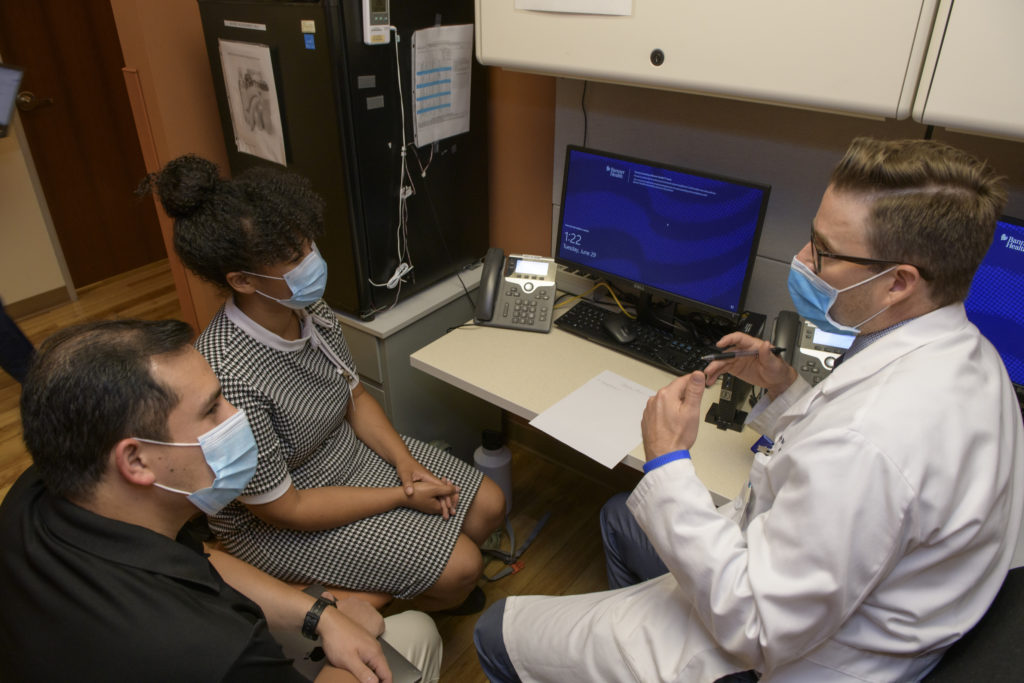
The UAHS end-of-life-care curriculum is among the first to be developed and then delivered using interprofessional collaboration by two or more disciplines. The training fills a gap locally, regionally and nationally, for training developed specifically for end-of-life care. While the evidence-based curriculum and toolkit will be developed with common cases, the training can be integrated into existing curricula and adapted to the needs of each discipline or learner.
In a survey of students from all four colleges, 75% said that end-of-life-care knowledge and skills were important to their future. “The students will be touched multiple times by the curriculum over their years of training,” said Mindy Fain, MD, Chief, Division of Geriatrics, General Internal Medicine and Palliative Medicine and Co-Director of the University of Arizona Center on Aging, a Board of Regents Center of Excellence. “We will be sharing the same cases and content across the UAHS disciplines to create a core set of shared knowledge, attitudes and actions to facilitate delivering the best of care as a unified team. We will be changing the healthcare culture with training that is relevant, impactful, and actionable. And we’re creating a healthcare workforce and a community where a majority of healthcare providers are engaged in advance care planning across the lifespan.”
The training aligns with the Institute for Healthcare Improvement Age Friendly Health System (AFHS) national initiative that the UA and Banner University Medical Center joined in 2019. “One of the pillars of an age friendly health system is the focus on the importance of asking patients what matters most to them,” said Dr. Fain. “The what-matters-most question can be what matters most to you in the clinic today, or what matters most to you as you look towards your upcoming surgery. We will train everyone on how to ask that question. And we will be eliminating the inconsistencies among the health care team in how they talk with each other and communicate with patients. This will make it easier for patients and families to make decisions as they deal with serious illness and approach end of life.”
Local community partners, including the Arizona End of Life Care Partnership and its members, have also contributed to design of the initiative. A part of the training is learning basic, culturally competent tools, and community resources available through the Partnership.
Dr. Fain concludes, “Fundamentally, the goal is to change how we talk, and to improve not only our comfort with it but to provide the language skill to talk about serious illness, death and dying. It’s not just having the conversation; we are changing care delivery and know that these conversations with patients and families improve health outcomes.”